The start of cold weather brings with it the Cold Season. Cases of viral respiratory infections start rising, causing missed school and work days. For families, this time of the year means sick kids at home, worried parents, and trying our best to recover. This article aims to share relevant facts and tips for parents to care for their families and themselves. It’s a long one, but I hope you find it helpful.
Consider downloading the guide with tips to take care of your immune system (click the button at the end of the article).
SOME FACTS
Healthy adults can have two to four colds per year. Children can have about six to ten colds for a year, but it can be as high as 12 in families with children at school.
Contrary to popular belief, cold weather doesn’t cause a cold. But, there are more colds during early fall to late winter. Most probably due to the following:
- These viruses may survive and reproduce more effectively at colder temperatures, making it easier for them to spread and infect more people.
- More indoor activities with closer proximity to each other, including school.
- Low humidity causes dry nasal passages to be more susceptible to cold viruses.
- Cold weather may also reduce the immune response and make it harder for the body to fight germs.
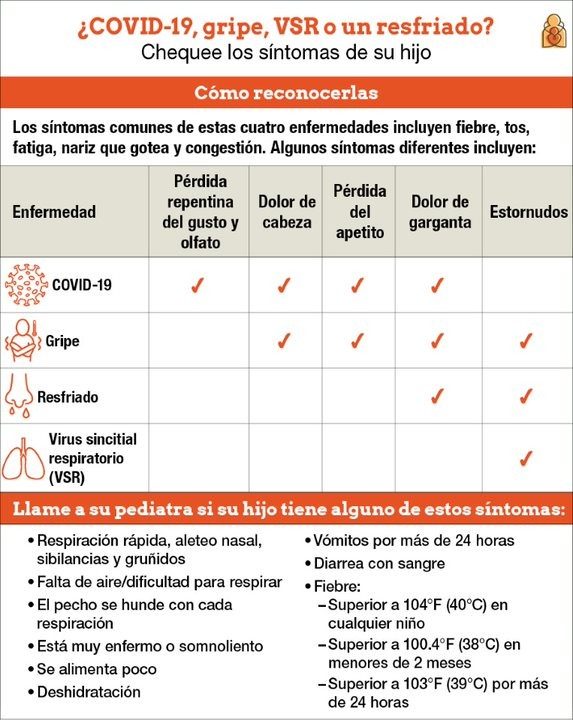
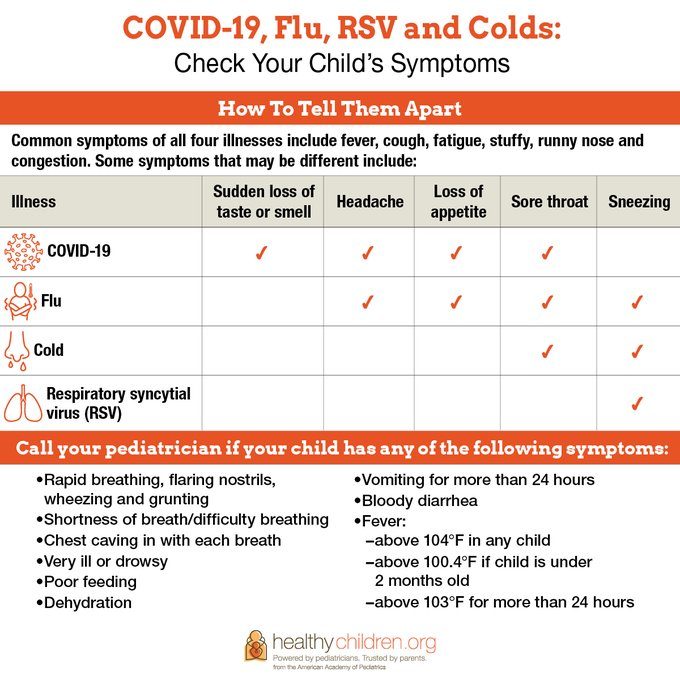
Check out these fantastic Infographics from the American Academy of Pediatrics’s website Healthychildren.org. A great reference to go back to if you or your kids get sick.
COMMON COLD
- There is no cure for the common cold.
- A virus causes it, so Antibiotics will not work to treat it.
- There are over 200 different viruses that cause the common cold.
- Rhinovirus is the most common one. Type A + B causes > 50% of common colds and affects the Upper Respiratory Airway (the nose, mouth, and throat). Type C causes a more severe infection, especially in kids. It involves the lower respiratory airway (trachea and lungs). It is commonly linked with asthma and chronic obstructive pulmonary disease (COPD) exacerbation and affects the lower respiratory airway (trachea and lungs).
How it is spread: it is very easily spread by airborne droplets that the sick person coughed or sneezed into the air. It can also spread when a sick person touches a surface or object someone else touches.
Incubation time*: 24 to 72 hours from exposure.
*The incubation period/time is between getting in contact with an infection and the appearance of the first symptoms.
How it starts: it varies from person to person, but most frequently with:
- Tinkle to a painful throat that lasts 1-2 days
OR
- Runny nose that starts watery and may get thicker and sticky. The standard color is white to yellow.
Duration: usually one week, but some may last two weeks.
Common Cold Complications: Colds can lead to secondary infections, including bacterial, middle ear, and sinus infections.
Special Note: Green phlegm or nasal discharge is usually related to bacterial infection. You or your child needs to be evaluated by a Healthcare Provider.
INFLUENZA or THE FLU
Flu A and B are the ones that cause seasonal epidemics. Flu C causes mild respiratory illness and no epidemic. Flu C affects cattle, and it’s not known to affect people.
Flu A causes fever + chills, cough, and fatigue.
Flu B causes sore throat, runny nose/stuffy nose, vomiting + diarrhea (more common in children), muscle and body aches, and headaches.
How it is spread: Similar to cold by air droplets and close contact with a sick person. Less by surfaces.
Incubation time: 1 to 4 days.
How it starts: Symptoms begin abruptly (common colds’ are gradual). People with flu are most contagious in the first three to four days after their illness begins.
Duration: most people recover in around two weeks.
Flu Complications:
Most cases are mild and do not need medical care. But, some people will develop complications, like:
- Sinus Infection
- Ear Infections
- Pneumonia: from either flu virus infection alone or co-infection of flu virus and bacteria
- Asthma attacks
- Myocarditis (inflammation of the heart)
- Encephalitis (inflammation of the brain) muscle tissues (
- Myositis, Rhabdomyolysis (inflammation of the muscle tissue), and
- Multi-organ failure (for example, respiratory and kidney failure).
Who are at risk for complications:
Children < 5 years old
Adults > 65 years old
Residents of nursing homes or long-term facilities
Pregnant women
American Indian and Alaskan
People with medical conditions:
- Decrease immunity (HIV, Cancer)
- Neuro or neurodevelopmental conditions
- Heart, Kidney, or Liver conditions
- Asthma
- Blood conditions
- Long-term aspirin use
- COPD
- Endocrinology problems
- Metabolic Problems
- Extreme obesity
RSV – Respiratory Syncytial Virus
- It’s a common respiratory virus that usually causes mild, cold-like symptoms.
- RSV is the most common cause of bronchiolitis (inflammation of the small airways in the lungs) and pneumonia (infection in the lungs) in US children younger than one year of age.
- This virus starts being around during fall and peaks in the winter.
- The seasonal patterns for this virus, and other common respiratory viruses, have changed since the start of the COVID-19 pandemic early in 2020. This virus appears during the spring and summer seasons (especially in the south of the US). Expert states it is too soon to predict if the previous pattern will return.
- RSV infections go away by themselves. The treatment goal is to relieve symptoms.
How it’s spread:
Coughing or sneezing from an infected person spreads virus droplets into your eyes/nose/mouth. Kissing a child’s face with RSV exposes you to the virus and touching surfaces that have it on them.
People infected are contagious for 3 to 8 days, especially 1 or 2 days before the first symptoms of illness.
Most kids are infected outside their homes in schools and childcare centers, bringing the virus home.
RSV survives many hours on hard surfaces like crib rails, toys, doorknobs, and tables.
Incubation time: 4 to 6 days.
How it starts: symptoms appear in stages, not all at once (check infographic). The only symptoms in babies may be irritability, less activity, and breathing problems.
Duration: the infection goes away in one or two weeks.
RSV Complications: severe infection causes bronchiolitis and pneumonia, especially in older adults and babies younger than six months. They may need hospitalization to help them with their breathing and treat dehydration. Other measures like additional oxygen or intubation may be necessary in the most severe cases. In most cases, the stay in the hospital lasts for a few days.
People at higher risk for complications:
- Premature babies.
- Young children with medical problems like heart and lung diseases, and weakened immunity.
- Adults with lung and heart disease or weakened immunity.
A mention of COVID-19:
RSV and COVID-19 are both contagious respiratory illnesses caused by different viruses, similar to the Flu and Common Cold viruses. They all share similar symptoms and are common causes of disease in children and adults.
COVID- 19 symptoms include fever, cough, fatigue, congestion, shortness of breath, sore throat, headache, sneezing, vomiting/diarrhea, or loss of taste/smell. These can appear 2 to 14 days after infection.
The best way to know if you have it is by testing. Some PCR tests can distinguish between Flu and COVID-19 at the same time, or they can be tested separately. Talk to a healthcare provider about getting tested for Flu and COVID-19 if you have symptoms.
Prevention is critical for all these infections.
- Help your immune system by eating healthy, exercising frequently, and sleeping well.
- Wash your hands often.
- Try to avoid close contact with sick people.
- Cover your nose and mouth with tissues or your elbow when coughing or sneezing. Teach your kids to do this.
- Avoid touching your eyes, nose, or mouth.
- Clean the surfaces in your home or workplace that you use more frequently for virus prevention.
- Talk to your Physician about getting vaccines.
How to treat them?
The best you can do to treat your children or yourself is to be as comfortable as possible while your body fights the infection.
Non-medical treatment:
Rest: this helps your body fight the infection.
Hydrate: plenty of fluids. Warm beverages usually help soothe sore throats. Consider reading these articles about hydration: Keeping Your Body Hydrated and How to Drink More Water and Keep Your Family Hydrated. You will find helpful information.
Warm steam: may help with congestion. Fill the bathroom with warm steam (from your shower), and have your kids or yourself stay inside for some minutes. Suction or make them blow their noses when congestion loosens up. Use bath time with the same purpose. Be vigilant to avoid burns with hot water.
Humidifier: your best help! Use a cool-mist humidifier (also called a vaporizer) in your and your children’s room. It helps the liquid in the stuffy nose get thinner and makes breathing easier. Place it close to you or your children (but safely out of reach). Make sure you carefully clean and dry the humidifier daily to stop bacteria or mold from growing, which can make you or your children sick. I have this one on my kids’ nightstands: Pure Enrichment MistAire Studio Ultrasonic Cool Mist Humidifier. It has four settings (including two with blues light) and lasts all night.
Warning: AVOID Hot-mist vaporizers. The hot steam can burn your child.
Nasal Spray (saline): helps with nasal congestion in all ages, especially babies (use saline drops). We use these two brands at home: Little Remedies Sterile Saline Nasal Mist and Boogie Baby Saline Nasal Spray Mist, Nasal Decongestant. These sprays are soft, so it doesn’t hurt inflamed little noses. My advice: stock up on this item; you will use it frequently.
Petroleum jelly for raw, chapped skin around the nose and lips
Cough:
Honey has proven to help with cough making it an excellent option for kids and avoiding cough medications.
- Do not give honey to babies under one year—it is unsafe.
- For children ages 1 to 5 years: half a teaspoon of honey.
- For children ages 6 to 11: one teaspoon of honey.
- For children 12 or older: two teaspoons of honey.
- If you give your kids honey at bedtime, ensure they brush their teeth afterward.
Medical treatment:
Caution: Infants and Children younger than four should not use over-the-counter medications. For older children, consult your Pediatrician before giving any medicine to get more information/recommendations.
Always call your Pediatrician before giving medicine to a child under two years of age, and call right away if your child is under three months of age and has a fever.
Pain and/or fever: analgesics and antipyretics like Ibuprofen and Acetominophen.
Nasal congestion: decongestant like Pseudoephedrine or Phenylephrine.
Cough: cough suppressants like Dextromethorphan and Diphenhydramine.
Cough and children: Cough drops or lozenges
- Do not give to kids younger than 4; they could choke on them.
- Do not give your children more cough drops than what the instructions on the package say.
Mentholated rubs
- For children ages two years and older: Rub a thick layer on top of the skin on the chest and the front of the neck (throat area).
- The medication goes into the air slowly, thanks to the body’s warmth. It helps to soothe a cough so that the child can sleep.
- Always put the medication container away and out of reach of the children.
- Only use mentholated rubs on the skin.
Chest congestion/mucous: expectorants like Guaifenesin.
Runny nose and sneezing: antihistamines (1st generation only) like Diphenhydramine.
If you choose to take medications for your symptoms:
Do not use two drugs to treat the same symptom.
Do not combine Guaifenesin (thins and loosens phlegm) AND Antihistamines (drys).
Read and follow labels carefully.
Double-check with your Doctor due to the risk of Side Effects if you:
- If you have Hypertension
- People 60 years old or older
- If you have a Stomach ulcer or gastritis
- If you take low-dose Aspirine for heart conditions
- If you have Asthma
- If you have a Cardiovascular Disease
- If you have a Kidney Disease
When to see your Doctor:
- Your symptoms last longer than two weeks.
- Your symptoms worsen, or you develop new symptoms, as you could have another type of infection.
- You have a sore throat or fever higher than 100 degrees for over three days.
- You’re experiencing intense chest pain and shortness of breath.
When to go to the Emergency:
Get medical care immediately if you or your child experience these symptoms!
In Children:
- Fast breathing or trouble breathing
- Bluish lips or face
- Ribs pulling in with each breath
- Chest pain
- Severe muscle pain (child refuses to walk)
- Dehydration (no urine for 8 hours, dry mouth, no tears when crying)
- Not alert or interacting when awake
- Seizures
- Fever above 104°F
- In children younger than 12 weeks, and fever
- Fever or cough that improves but then returns or worsens
- Worsening of chronic medical conditions
In Adults:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest or abdomen
- Persistent dizziness, confusion, inability to arouse
- Seizures
- Not urinating
- Severe muscle pain
- Severe weakness or unsteadiness
- Fever or cough that improves but then returns or worsens
- Worsening of chronic medical conditions
Please consult your Doctor for any other concerning or severe symptoms, especially in children.

Key points to take home:
- All the mentioned viruses cause inflammation of the membranes that line the nose and throat. Some of them can cause complications.
- These viruses (especially the ones causing Common Colds) easily spread to others. Often spread through airborne droplets that a sick person coughed or sneezed into the air. Another person then inhales the droplets. Remember about surface contamination as well.
- They all have similar symptoms, including a stuffy, runny nose, scratchy, tickly throat, sneezing, watery eyes, and a low-grade fever. Review the infographics above.
- Treatment to reduce symptoms includes resting and drinking plenty of fluids. Infants and Children younger than four should not be given over-the-counter medications without consulting their Pediatrician.
- Because viruses cause colds, treatment with antibiotics won’t work.
- The best prevention is frequent hand washing and avoiding close contact with sick people.
- Talk to your doctor about getting the vaccines for Flu and COVID-19.
- The only way to know if you have COVID-19 or FLU is to get tested.
- A strong immune system goes hand to hand with a healthy body. Following a healthy lifestyle will help you get sick less often, and if you get sick, to recover faster and avoid complications.
Are you ready to help your Immune System work its best?
Get my Free Guide now and start working on it.
Click below to get it.
Remember to Subscribe to My Newsletter to don’t miss a thing! I promise not to fill up your mailbox.
Disclosure:
This article is for informational and educational purposes only. It is not, nor is it intended to be a substitute for professional medical advice, diagnosis, or treatment and should never be relied upon for specific medical advice.
This post contains affiliate links. I may earn a small commission if you purchase at no additional cost to you. I only share products or services I and/or my family personally use and recommend!
I value your privacy. I use cookies and other technologies to keep the site reliable and secure, tailor your experience, measure site performance, and present relevant offers and advertisements, as described in my Privacy Policy (here).






